Tracheotomy and Ventilation |
|
|
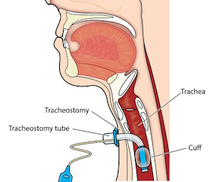
Some people living with ALS choose to extend their lives by deciding to receive invasive ventilation. This involves a surgical procedure called a tracheotomy that creates an opening in your neck where a tube connects to a ventilator that will breathe for you.
It is very important to learn about and discuss this option ahead of time with your loved ones and ALS professionals. Going on full-time mechanical ventilation can help you live longer, but it can also come at a great cost to you and your family. It does not slow down disease progression or reverse ALS. |
|
|
Learn about respiratory challenges, monitoring, support, intervention, equipment, and more in our comprehensive ALS Respiratory Guide.
|
Should I get a tracheotomy?This is a very personal decision. Only you and your family will know what is best. This is a decision that cannot be reversed. If you are considering getting a tracheotomy, discuss the pros and cons with your neurologist, ALS clinic team, and local ALS organization.
|
|
It is important to talk with your loved ones because once you are on invasive ventilation, you will need 24/7 assistance. Professional skilled home care is expensive and not covered by Medicare. Most families cannot afford full-time professional care, which means family members often become full-time caregivers.
Common reasons for not getting a tracheotomy include financial cost, burden to family members, and concerns about living a diminished quality of life. The vast majority of trached ALS patients remain attached to their ventilators 24/7 and are unable to speak.
Reasons for getting ventilated include the desire to continue living, spending more time with loved ones, and fulfilling a greater purpose. Advancements in respiratory and communication technology have enabled people to be more comfortable, stay connected, and have a better quality of life.
Common reasons for not getting a tracheotomy include financial cost, burden to family members, and concerns about living a diminished quality of life. The vast majority of trached ALS patients remain attached to their ventilators 24/7 and are unable to speak.
Reasons for getting ventilated include the desire to continue living, spending more time with loved ones, and fulfilling a greater purpose. Advancements in respiratory and communication technology have enabled people to be more comfortable, stay connected, and have a better quality of life.
“I thought of our youngest son, and that I owed it to him to be around, if I could, for his high school graduation, or college graduation, and for our youngest daughter, to maybe see her get married. Suddenly it wasn't about me, it was about them.
"[Ventilation] is really not that bad! It takes some getting used to, no doubt, but if you take it a day at a time, or a minute at a time, you get through it, you adapt. One plus is that you can finally breathe. My family and friends say that I look 100% better than I did, and I have five times the energy.”
– Tim Green, former NFL player living with ALS
"[Ventilation] is really not that bad! It takes some getting used to, no doubt, but if you take it a day at a time, or a minute at a time, you get through it, you adapt. One plus is that you can finally breathe. My family and friends say that I look 100% better than I did, and I have five times the energy.”
– Tim Green, former NFL player living with ALS
When should I get a tracheotomy?
|
When your respiratory muscles weaken to the point that noninvasive ventilation no longer provides enough breathing support, you can get a tracheotomy so that a ventilator will breathe for you.
Learn about your options ahead of time so you fully understand what your decision entails. Talk with medical professionals, ask questions, and discuss with the loved ones who would be involved in your care. Once you make a decision, be sure to update your advance directives so that your wishes are clear to loved ones and medical professionals. If you change your mind later, you can always go back and update your advance directives. |
|
What is the surgical procedure like?
|
If you are considering a tracheotomy, your neurologist will refer you to a pulmonologist for consultation. The pulmonologist can answer all of your questions regarding the procedure and rehabilitation.
Getting a tracheotomy is much more involved than getting a feeding tube. ALS patients often remain in the hospital for two to four weeks after a tracheotomy. You will need to go to a rehab facility to learn how the ventilator works, and your personal caregivers will need to be trained before you go home. |
|
Once I have a tracheotomy, how does it work?
At home, you will be attached to a portable ventilator, which will breathe for you. Your caregivers will know how the machine works and will need to make sure that it is working properly. Most ALS patients will be on the ventilator 24/7, though some patients can disconnect for short periods of time during the day.
In most cases, once you are on a ventilator, you will need to get your nutrition, liquids, and medication through a feeding tube. If you do not already have a feeding tube, you will receive one when you are under anesthesia for the tracheotomy procedure.
In most cases, once you are on a ventilator, you will need to get your nutrition, liquids, and medication through a feeding tube. If you do not already have a feeding tube, you will receive one when you are under anesthesia for the tracheotomy procedure.
What if I decide to stop using the ventilator?
|
If you decide to disconnect the ventilator, your breathing will take its natural course. If your respiratory muscles are greatly weakened, then your breathing will likely slow before stopping altogether.
Patients who decide to go this route often bring hospice care into the home and receive sedation before removing the ventilator, which can help minimize breathing distress and provide a more comfortable end-of-life experience. |
|
Is this procedure expensive?
Ask your medical providers to give you an estimate ahead of time for what you will need to pay out of pocket. The most expensive part is usually the 24/7 assistance you will need once you are home. Medicare will not cover long-term home care if you are on a ventilator, and most insurance policies won’t either. If family and friends cannot provide full 24/7 coverage, paying for a trained caregiver or skilled nursing care can be very expensive.
What if I decide not to get a tracheotomy?
If you decide against the procedure, you can continue to use a portable ventilator (Trilogy) for noninvasive breathing support. If you reach the point where you are struggling to breathe, hospice can administer drugs to provide a more comfortable end-of-life experience.
ALS Medical Decisions
|
|