|
When her husband was diagnosed with ALS five years ago, Lori met with clinicians and researchers across the country to find the best care for her husband. Since then, she has been a fierce advocate for the entire ALS community.
Lori serves on the core advisory team for I AM ALS, works on multiple committees at NEALS, and raises money for expanded access programs. She also moderates discussions on her popular This Is ALS Facebook group. |
What were your lives like before your husband’s symptoms?
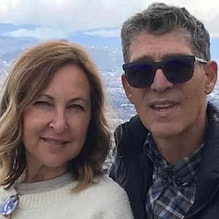
My husband Brian and I have been married for almost 40 years. We're actually high school sweethearts. So we've basically grown up with each other starting at the age of 16 when we started dating. We live in Chicago. I have a family-run business that I've been running for the last 40 years with my husband. And we raised three children here in Chicago and they're all grown men now. And we are proud to say we're grandparents.
|
Brian was diagnosed five years ago with sporadic ALS. You're never really prepared to receive a diagnosis with the three letters “ALS”. When we were diagnosed five years ago, we felt like our lives stood still for a moment. But then we kicked into, "Okay, what do we have to do? Where do we need to go? What drugs are out there? What therapies are effective?”
|
|
We didn’t know much about the disease, other than reading Tuesdays with Morrie and thinking to myself over the years, "God, I would never want to have to be confronted with a disease like ALS. It just sounds so terrible, and it's so terminal."
Not knowing much about the disease and having to educate ourselves was definitely a challenge, but we felt fortunate that we had the resources to explore all sorts of clinicians around the country to figure out who could best advocate for us from a clinical standpoint. And so we did this nationwide tour of meeting all the different clinicians across the country.
Not knowing much about the disease and having to educate ourselves was definitely a challenge, but we felt fortunate that we had the resources to explore all sorts of clinicians around the country to figure out who could best advocate for us from a clinical standpoint. And so we did this nationwide tour of meeting all the different clinicians across the country.
What were Brian’s initial symptoms?
My husband has always been incredibly physically fit. He played every sport, and every sport he played, he played well. So being an athlete, he was very tuned into his body. He had been working out with the same trainer for a number of years and noticed that he was suffering from some weakness and couldn't lift the same amount of weight on his left side. So he went to a neurologist who said they’d do an MRI to see what was going on.
The neurologist came back to us and said, "There's a little impingement that I see on your spine, but I'll send you to a neurosurgeon. They can fix it. Boom, you'll be fine. You'll be able to resume life as it was before."
My husband didn’t want to go that route. He didn’t want anyone operating on him. So he tried physical therapy for a while. Things weren't getting any better, but they weren't getting any worse. So he just stopped physical therapy and adapted his workouts.
So then we sort of lived with this weakening on the left side and didn't really think anything of it. And then about a year and a half later, we were in Washington, DC and I noticed that when my husband was walking long distances, he seemed to have a slight limp, as though something wasn't firing properly. And he said the same thing. Normally we could walk for hours and hours, but I noticed he was slowing down.
The neurologist came back to us and said, "There's a little impingement that I see on your spine, but I'll send you to a neurosurgeon. They can fix it. Boom, you'll be fine. You'll be able to resume life as it was before."
My husband didn’t want to go that route. He didn’t want anyone operating on him. So he tried physical therapy for a while. Things weren't getting any better, but they weren't getting any worse. So he just stopped physical therapy and adapted his workouts.
So then we sort of lived with this weakening on the left side and didn't really think anything of it. And then about a year and a half later, we were in Washington, DC and I noticed that when my husband was walking long distances, he seemed to have a slight limp, as though something wasn't firing properly. And he said the same thing. Normally we could walk for hours and hours, but I noticed he was slowing down.
How did he get diagnosed?
When we got back from Washington, I asked a physician friend of mine to see Brian. After the exam, she called me and said, "Clinically, he seems really strong, but there's something going on. I think we need to do an EMG to figure out where the weakness is coming from. A couple of days later she called me and said, "I don't want to prognosticate, but I'm concerned that there is something in fact going on with Brian. But I need to refer you out to a neurologist at Northwestern." At the time, she didn't tell me this, but the neurologist she referred us to was a neurologist at the ALS clinic.
So we made an appointment and repeated the EMG. Those results confirmed that it was ALS. We didn't stop there though, because we felt as though we needed to go and speak to other clinicians and researchers around the country, which we did.
We eventually ended up at Mass General, where we met Dr. Merit Cudkowicz. She also gave an official diagnosis after doing some tests. And that was it. And so that took two years from symptom onset to an official diagnosis.
So we made an appointment and repeated the EMG. Those results confirmed that it was ALS. We didn't stop there though, because we felt as though we needed to go and speak to other clinicians and researchers around the country, which we did.
We eventually ended up at Mass General, where we met Dr. Merit Cudkowicz. She also gave an official diagnosis after doing some tests. And that was it. And so that took two years from symptom onset to an official diagnosis.
What types of tests did they run?
The way they get to their diagnosis is sort of an exclusion process. They rule out everything else before they even test for ALS. So they tested my husband for Lyme disease, for other neurodegenerative diseases, for MS. So basically they tested him for everything until they finally tested him for ALS, which was the EMG. And that was the definitive test that gave us the diagnosis. He’d had numerous EMGs, a spinal tap, and some genetic testing. But at the end, the EMG is really what gives the clinicians the final diagnosis of ALS.
How did you get the news?
Well, that's a really interesting question, because a couple of days after we had gone to Northwestern, I got a notification in my email that our test results were on the MyChart platform. I went in and I started reading it and thought, "Okay, what is lower motor neuron disease?" And then, "Oh God, this is not going to be good."
I immediately copied and pasted the words to my brother, who is a physician. He called me immediately. But the line went silent. He couldn't speak. And then all of a sudden I heard this sort of outpouring of tears and crying. And he said, "Lori, Brian has ALS." And it was like, "What? I received the news via email in a note in MyChart. That's how I received the news?"
So you can imagine when I read that and I was having this conversation with my brother, he was just beside himself. So that is how I officially received the news—instead of having a sit-down conversation with our clinician at Northwestern. So it was tough. It was very, very tough.
You don't want to receive a diagnosis like that via an email. I did have a long conversation with my brother, who gave us suggestions, started looking into therapies, and spoke with some of his colleagues. But basically, the answer is always the same: You have three to five years to live.
I immediately copied and pasted the words to my brother, who is a physician. He called me immediately. But the line went silent. He couldn't speak. And then all of a sudden I heard this sort of outpouring of tears and crying. And he said, "Lori, Brian has ALS." And it was like, "What? I received the news via email in a note in MyChart. That's how I received the news?"
So you can imagine when I read that and I was having this conversation with my brother, he was just beside himself. So that is how I officially received the news—instead of having a sit-down conversation with our clinician at Northwestern. So it was tough. It was very, very tough.
You don't want to receive a diagnosis like that via an email. I did have a long conversation with my brother, who gave us suggestions, started looking into therapies, and spoke with some of his colleagues. But basically, the answer is always the same: You have three to five years to live.
After the initial shock, what did you do?
|
When we received the diagnosis, our lives sort of stood still. It's a hard diagnosis to digest. Just because you know that there are really no cures or treatments. It's not like you get a cancer diagnosis and you're starting on meds, or you enroll immediately into a clinical trial. Or there are therapies out there that can sort of hold things at bay that might be effective.
|
|
Knowing that there are no cures is something that was very, very difficult for us to comprehend. I said, "We're going to get to work. We're going to speak to people. We're going to find what's out there. We're going to find the effective treatments and therapies. We're not going to let this disease define us. We're going to move forward like we do with our business, with any hurdles that we are faced with. We find that there are always solutions and workarounds.”
And so that was my mentality: "Let's leave no stone unturned, no grain of salt unturned. Let's research this to death. Let's find out what's out there, let's do this. Let's find something." And that's sort of how we've been ever since then, in terms of our advocacy work, in terms of helping other patients who received the diagnosis, working closely with clinicians in this field, working to be fierce advocates—not only for my husband, but for the entire community.
I always want to be in the know, I want to know what's going on, I want to know all the facts. That's my personality. It's not my husband's personality at all. I'm always the step in, take charge kind of person. I figure if there's a problem, I can resolve it. That’s how I approach life in general, having run a business for 40 years and having raised children. It's my tenacity. It's also not giving up easily. My mantra is, "My husband's going to die with the disease, not from the disease.”
With any diagnosis that you get, especially with ALS, you don't want to curl up and die. You want to pick yourself up by your bootstraps and move forward, and do whatever you can in the best way you can to continue to live a full life—and also cling onto this hope that there will be a treatment, a therapy in the near future that can help not only Brian, but everybody else in this community.
And so that was my mentality: "Let's leave no stone unturned, no grain of salt unturned. Let's research this to death. Let's find out what's out there, let's do this. Let's find something." And that's sort of how we've been ever since then, in terms of our advocacy work, in terms of helping other patients who received the diagnosis, working closely with clinicians in this field, working to be fierce advocates—not only for my husband, but for the entire community.
I always want to be in the know, I want to know what's going on, I want to know all the facts. That's my personality. It's not my husband's personality at all. I'm always the step in, take charge kind of person. I figure if there's a problem, I can resolve it. That’s how I approach life in general, having run a business for 40 years and having raised children. It's my tenacity. It's also not giving up easily. My mantra is, "My husband's going to die with the disease, not from the disease.”
With any diagnosis that you get, especially with ALS, you don't want to curl up and die. You want to pick yourself up by your bootstraps and move forward, and do whatever you can in the best way you can to continue to live a full life—and also cling onto this hope that there will be a treatment, a therapy in the near future that can help not only Brian, but everybody else in this community.
How has Brian’s ALS progressed?
|
When you're given the diagnosis, they tell you, "Get your affairs in order, check everything off your bucket list, and try to live your life to the fullest, because ALS is a terminal disease.”
We're five years into the disease right now. And whenever I tell people that they're like, "Oh my God, five years. That's incredible." And so it truly is amazing that my husband is still really high functioning today. |
|
But five years ago, if you would've asked me that, I would have never been able to say those words, that he is still five years in, doing well and living a very full life. As you know, once you're given a diagnosis like that, it's a diagnosis of finality and you feel like, "Okay, our lives are coming to an end now, and what do we need to do to live a very full life in just the three years that you're given to live.”
So we feel very fortunate on many different levels. A lot goes back to our relationship, our supportive family, and our advocacy work, which fills our days and gives us a lot of hope knowing that there's a community out there that is working towards finding cures.
So we feel very fortunate on many different levels. A lot goes back to our relationship, our supportive family, and our advocacy work, which fills our days and gives us a lot of hope knowing that there's a community out there that is working towards finding cures.
What types of treatments does Brian take?
Brian does what everybody else does, like taking riluzole and all of the standard over-the-counter therapies like inosine, Basis, and TUDCA. He's also on Radicava and we do infusions at home. And then he is also taking RT001 on an EAP through the Healey Center.
There's no real understanding or answer that I could give you about why Brian is doing so well. Typically, by year five, you're sort of at the end stages of your life. ALS is such a complex disease that the clinicians and researchers really don't have any idea why Brian is such a slow progressor. But there's probably 5% of people who can live 10 years or more with this disease. And we're obviously hoping Brian falls into that bucket.
There's no real understanding or answer that I could give you about why Brian is doing so well. Typically, by year five, you're sort of at the end stages of your life. ALS is such a complex disease that the clinicians and researchers really don't have any idea why Brian is such a slow progressor. But there's probably 5% of people who can live 10 years or more with this disease. And we're obviously hoping Brian falls into that bucket.
Does anyone know why it’s progressing so slowly?
No one really knows, but we'll take it. In the last year, our neurologist wanted to retest Brian with another EMG. And this time she was very specific as to what the technician should be looking for.
We were hoping she would say something different, but she did confirm it as ALS. But again, a very, very slow course. She doesn't know why he's been on this plateau for many years. Is it just Brian? Is it what he's doing? Is it the fact that he's still working out? No one really knows.
We were hoping she would say something different, but she did confirm it as ALS. But again, a very, very slow course. She doesn't know why he's been on this plateau for many years. Is it just Brian? Is it what he's doing? Is it the fact that he's still working out? No one really knows.
Does Brian still exercise?
People say that when you have this disease, you can tire really quickly. And it doesn't matter how many reps you do or how much weight you lift because you're not going to get stronger. Obviously in this disease, you continue to get weaker. But Brian tries to just maintain good health and exercise. He notices that when he doesn't exercise, he starts to feel more tired, more crampy. So it's better for him when he does exercise. And he exercises approximately three days a week.
Twice a week, he works with a trainer who he's worked out with for over 20 years. And they just adapt. You do modifications, you adapt to how you're feeling that particular day. And that seems to be working out really well for Brian. And then he still rides his bike, and he still plays tennis. These are all things that he's grown up with that he doesn't want to have to give up while he can still do them, with modifications obviously. So he's going to still stay the course and do what he can, how often he can. (Learn more about ALS and exercise.)
Twice a week, he works with a trainer who he's worked out with for over 20 years. And they just adapt. You do modifications, you adapt to how you're feeling that particular day. And that seems to be working out really well for Brian. And then he still rides his bike, and he still plays tennis. These are all things that he's grown up with that he doesn't want to have to give up while he can still do them, with modifications obviously. So he's going to still stay the course and do what he can, how often he can. (Learn more about ALS and exercise.)
Has he enrolled in clinical trials?
Unfortunately, my husband wasn't a candidate for clinical trials. Enrollment into clinical trials can be a very frustrating process for people. There are many hurdles and many exclusions into getting into trials.
I keep hearing from patients that their clinicians have never really spoken to them about clinical trials. And we don't really know why because there are plenty of resources out there for patients to find out about clinical trials.
I think that, first and foremost, we need to better inform and educate our clinicians so they can have these conversations with patients who are newly diagnosed. I think that things have definitely gotten better. There are, I think, 80 trials around the country now that are enrolling. I think we need to look at clinical trials right from the onset of diagnosis to be able to explore the possibilities of enrolling.
We want to have effective treatments and cures, and how do we get there? We get there with science—and clinical trials are solely science. But from a patient's perspective, it does bring us a sense of hope.
I think people enroll in clinical trials for two reasons. One is strictly for science, the other is, "I'm hopeful they’re going to find a cure one day and I want to be part of it. I might get the placebo, but there is a 50/50 chance that I may get the drug." If we have 50% hope for the chance of getting in, let's do it. Why not? I mean, that's my philosophy. Science is important and we need that information to help move the ball forward.
I keep hearing from patients that their clinicians have never really spoken to them about clinical trials. And we don't really know why because there are plenty of resources out there for patients to find out about clinical trials.
I think that, first and foremost, we need to better inform and educate our clinicians so they can have these conversations with patients who are newly diagnosed. I think that things have definitely gotten better. There are, I think, 80 trials around the country now that are enrolling. I think we need to look at clinical trials right from the onset of diagnosis to be able to explore the possibilities of enrolling.
We want to have effective treatments and cures, and how do we get there? We get there with science—and clinical trials are solely science. But from a patient's perspective, it does bring us a sense of hope.
I think people enroll in clinical trials for two reasons. One is strictly for science, the other is, "I'm hopeful they’re going to find a cure one day and I want to be part of it. I might get the placebo, but there is a 50/50 chance that I may get the drug." If we have 50% hope for the chance of getting in, let's do it. Why not? I mean, that's my philosophy. Science is important and we need that information to help move the ball forward.
How are EAPs related to clinical trials?
An EAP is an expanded access program that can help patients like Brian, who can't enroll in clinical trials. So the EAP is an opportunity for patients to get on certain drugs that are testing in trial or not starting yet in trial. It’s more of an experimental thing. So you're actively getting the drug, but you don't really know what the effect will be.
But there is that opportunity for patients, and clinicians should offer those opportunities also because at different sites there are EAPs available. Brian, for example, is in the RT001 EAP, which is a very small EAP, but the drug company has produced and allowed certain patients outside of the trial to try the drugs. And so EAPs also bring another sense of hope if you can't get into a trial. You can have this conversation with your clinicians to find out what companies are making EAPs available for patients who have been excluded from clinical trials.
So more and more now, as an advocacy group, we're demanding EAPs. We need these pharmaceutical companies to produce enough drugs for those individuals who are not eligible for trials to have access to drugs.
But there is that opportunity for patients, and clinicians should offer those opportunities also because at different sites there are EAPs available. Brian, for example, is in the RT001 EAP, which is a very small EAP, but the drug company has produced and allowed certain patients outside of the trial to try the drugs. And so EAPs also bring another sense of hope if you can't get into a trial. You can have this conversation with your clinicians to find out what companies are making EAPs available for patients who have been excluded from clinical trials.
So more and more now, as an advocacy group, we're demanding EAPs. We need these pharmaceutical companies to produce enough drugs for those individuals who are not eligible for trials to have access to drugs.
What is I AM ALS, and how can people get involved?
|
I AM ALS is a patient-centric, patient-driven organization. It's solely run by patients and caregivers, and advocates who are doing everything that we possibly can in addressing every aspect of this disease in order to help give people the resources and tools they need to live with ALS. The patient navigation portal is invaluable because we've collected so much information that is so helpful that when people call in, we can give them the information that they can then go access. We've never had that before.
|
|
And that in itself is such a gift, knowing that there are people there that can connect with the organization and then feel empowered enough to go out and do something to then become advocates themselves and get involved, or to just know what resources are out there. It's a great way to reach out to people to get answers to your questions on a timely basis. And then to take that information, and feel empowered to do something.
At the end of the day, we need more advocates in this disease, we need more people involved. We need people to help spread awareness and to educate people, because as we know, a lot of people still don't know what ALS is. From a personal perspective, my advocacy work is sort of my form of self care, knowing that I'm doing things that are good for the community. I enjoy interacting with people and networking. I enjoy offering information and resources.
I think that we've seen the power of the patient, we've seen what changes we can make in order to improve the lives of people living with ALS and family members. And I think now it's fair to say that we as a group need to be seated at the table when speaking to legislators, FDA, NIH, clinicians, contract research organizations, and pharmaceutical companies. We are demanding to be partners in this process. And I think that that is really, really powerful and really impactful.
At the end of the day, we need more advocates in this disease, we need more people involved. We need people to help spread awareness and to educate people, because as we know, a lot of people still don't know what ALS is. From a personal perspective, my advocacy work is sort of my form of self care, knowing that I'm doing things that are good for the community. I enjoy interacting with people and networking. I enjoy offering information and resources.
I think that we've seen the power of the patient, we've seen what changes we can make in order to improve the lives of people living with ALS and family members. And I think now it's fair to say that we as a group need to be seated at the table when speaking to legislators, FDA, NIH, clinicians, contract research organizations, and pharmaceutical companies. We are demanding to be partners in this process. And I think that that is really, really powerful and really impactful.
Do you have any overarching advice for fellow caregivers?
I think it's really important, if you feel comfortable, to put yourself out there in the community and have conversations with other patients and caregivers and feel comfortable enough to ask the types of questions that you don't know the answers to. Getting the information direct from the source is always a good thing as opposed to going about it in a roundabout way.
Get involved in the community, explore other organizations that offer resources and helpful information, and collect all the information you possibly can. And then take the necessary steps that you think you should take in order to help better things in your lives.
Get involved in the community, explore other organizations that offer resources and helpful information, and collect all the information you possibly can. And then take the necessary steps that you think you should take in order to help better things in your lives.
This Is ALS
|
Lori Andre moderates a Facebook group for people living with ALS, caregivers, family, and friends. It is a good place to stay up to date on ALS news, get answers to your questions, and connect with others facing similar challenges. Watch this video to learn more. Visit the This Is ALS page to join.
|
|